Processing Your Payment
Please do not leave this page until complete. This can take a few moments.
-
News
-
Editions
-
- Lists
-
Viewpoints
-
HBJ Events
-
Event Info
- 2024 Economic Outlook Webinar Presented by: NBT Bank
- Best Places to Work in Connecticut 2024
- Top 25 Women In Business Awards 2024
- Connecticut's Family Business Awards 2024
- What's Your Story? A Small Business Giveaway 2024 Presented By: Torrington Savings Bank
- 40 Under Forty Awards 2024
- C-Suite and Lifetime Achievement Awards 2024
- Connecticut's Health Care Heroes Awards 2024
-
-
Business Calendar
-
Custom Content
- News
-
Editions
View Digital Editions
Biweekly Issues
- April 29, 2024
- April 15, 2024
- April 1, 2024
- March 18, 2024
- March 4, 2024
- February 19, 2024
- February 5, 2024
- January 22, 2024
- January 8, 2024
- + More
Special Editions
- Lists
- Viewpoints
-
HBJ Events
Event Info
- View all Events
- 2024 Economic Outlook Webinar Presented by: NBT Bank
- Best Places to Work in Connecticut 2024
- Top 25 Women In Business Awards 2024
- Connecticut's Family Business Awards 2024
- What's Your Story? A Small Business Giveaway 2024 Presented By: Torrington Savings Bank
- 40 Under Forty Awards 2024
- C-Suite and Lifetime Achievement Awards 2024
- Connecticut's Health Care Heroes Awards 2024
Award Honorees
- Business Calendar
- Custom Content
Here’s how some nursing homes and assisted-living facilities blocked COVID-19 spread
 PHOTOS | STEVE LASCHEVER
Heidi Lubetkin, vice president of clinical support services at The Retreat in Hartford, says the assisted-living facility’s immediate response to the COVID-19 outbreak has kept all of its residents safe.
PHOTOS | STEVE LASCHEVER
Heidi Lubetkin, vice president of clinical support services at The Retreat in Hartford, says the assisted-living facility’s immediate response to the COVID-19 outbreak has kept all of its residents safe.
Before COVID-19 began to spread across Connecticut in early March, The Retreat in Hartford took several precautionary steps, including going into immediate lockdown.
The affordable assisted-living facility’s early and aggressive reaction is likely why none of its 100 low-income seniors or 100 staffers have contracted coronavirus, despite the disease running rampant in other nursing homes and senior-care facilities across the state, said Heidi Lubetkin, who has been the vice president of clinical support services at The Retreat since its inception more than 15 years ago.
“We skipped all the [response] steps and immediately went to the high-risk level,” said Lubetkin. “Many [elderly care] facilities were electing to select the low-risk response at that point.”
The Retreat, located across the street from Hartford Hospital, in early March also restricted visitation and the use of common areas, and began stockpiling personal protective equipment (PPE). The facility, operated by nonprofit human-services organization Community Renewal Team (CRT), also improved its air filtration systems, started hourly cleanings of high-touch surfaces and furloughed a third of its staff to reduce exposure in its seven-story building.
“If we hadn’t locked ourselves down until maybe residents were starting to cough, that would have ended up being like a match in our building,” she said.
The Retreat is among the dozens of Connecticut assisted-living facilities and nursing homes that have prevented the novel coronavirus from entering their doors, and the safety precautions they took offer clues into how to contain the spread of the deadly disease in senior-care facilities, which have experienced major COVID-19-related deaths and outbreaks.
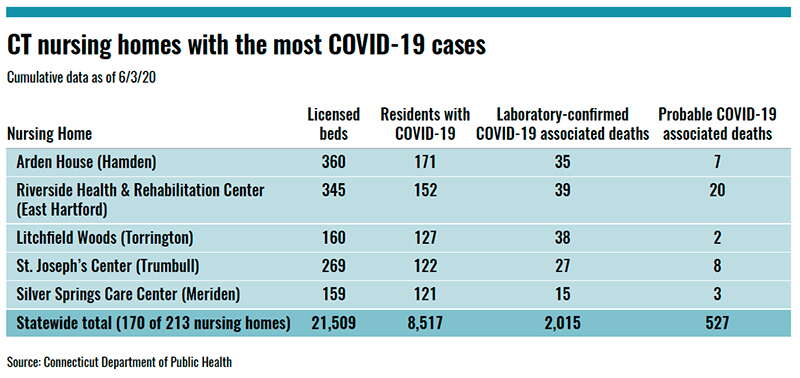
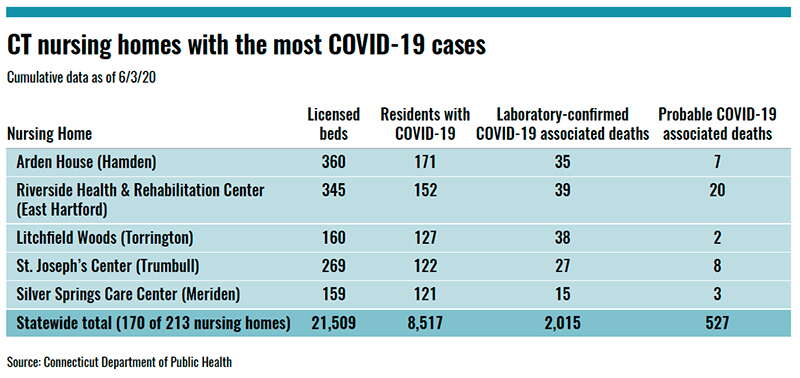
The fact that nursing homes and assisted-living facilities have accounted for more than half of the state’s 4,100 COVID-19-related deaths — and more than 20% of all coronavirus cases — has set off alarm bells and forced Gov. Ned Lamont to call for an independent, third-party review of the industry’s preparation and response to the pandemic.
Questions remain over why nursing home staff were not initially subject to widespread testing, and why government inspectors found infection control problems in one out of every four Connecticut nursing homes they examined prior to June 3. There is also a lack of clarity over why Connecticut facilities with more black and Latino residents have been hit harder by the outbreak compared to those where the population is mainly white.
Finding answers to those questions could be the key to readying Connecticut for the next public health emergency, officials say.
The good news, though, is that death and infection rates at long-term care facilities have slowed in recent weeks, allowing some nursing homes to begin loosening visitor or other restrictions.
“As we prepare for the possibility of a second wave, we must be proactive in analyzing what occurred, what needs to be improved, and how we can ensure the quality and safety of facilities that some of our most vulnerable residents call home,” the governor said in announcing the third-party review of senior-care facilities.
As The Retreat started to learn more about the severity of the COVID-19 outbreak, it implemented the Centers for Disease Control and Prevention’s mitigation plan for nursing homes on March 10, instead of waiting for the state’s guidance that came weeks later.
CDC’s infection prevention and control program offers low-, medium- and high-risk response plans for sites as needed.
The Retreat, Lubetkin says, took the urgent step of selecting the high-risk level right away because that was being used as a blueprint for nursing homes, which are regulated more tightly by federal and state governments and have more access to PPE.
“It helped to give us guidance because [assisted-living facilities] unfortunately are still not guided as best as we can be,” she said. “So it was kind of up to us to come up with this plan.”
The high-risk plan forced The Retreat, which provides behavioral health and addiction services to certain fixed-income residents ages 65 and older, to reconsider visitation, food service, sanitation, ventilation and even laundry service.
New rules included making sure employees aren’t working at multiple sites, and that they had enough PPE to protect themselves outside of business hours.
The Retreat has shut down community dining areas for several months and instead delivers food directly to residents’ rooms twice a day to limit exposure from outside environments.
It also sterilizes mail before it enters the building; provides temperature checks for residents and visitors; uses staggered shifts; holds outdoor staff meetings; uses telehealth and modified laundry services; and provides videoconferencing and limited outdoor seating for residents to visit with family and friends.
“We try to have as much fun as possible because it’s a marathon and it’s not ending anytime soon,” Lubetkin said.
Vernon Manor, an independently owned and privately managed nursing home in Vernon, is another long-term care facility that recently reported all of its 100 or so residents and 180 employees tested negative for COVID-19.
The two-story nursing home, serving mainly Medicaid recipients originally from eastern Connecticut, also took immediate action following CDC guidelines in mid-March, according to Administrator Angela Perry.
For example, Perry said it required universal face-coverings for staff, secured a three-month supply of PPE and completed so-called point prevalence surveys that involved testing all residents. State health and nursing home officials say this is a vital data-collection tool that can be used to control the potential spread of infection.
Other precautions include installing small, portable air filtration systems in high-traffic common areas; hiring an outside vendor to boost in-house cleaning services; limiting community activities; supplying PPE to staff; and collaborating with other facilities on best practices.
Residents were even educated on the health benefits of social distancing during the pandemic.
“I think what really led us to not having any cases to date is we implemented practices early on,” Perry said.
It’s still not fully clear why the virus transmits more at certain nursing homes or assisted-living facilities, said Matthew Barrett, president and CEO of the Connecticut Association of Health Care Facilities (CAHCF), which represents assisted-living facilities and for-profit nursing homes in the state.
Barrett said a lack of nationwide understanding about asymptomatic transmission of COVID-19 earlier this year played a key role in cases spiking at senior-care facilities. The lack of testing capacity and PPE early on also contributed to the country’s late response, he said.
But that still doesn’t fully explain why some nursing homes have zero cases and others have been hit hard, including the Arden House in Hamden, which has reported 171 residents with COVID-19, said Barrett, who recently supported Lamont’s call for an independent review.
With the majority of facilities implementing symptom-based strategies and regulations, he said many of CAHCF’s nursing home and assisted-living facility members have wondered whether density of population and the presence of COVID-19 within that group is a driving force behind a spread.
“Everyone has implemented a severe visitor restriction, temperature checking, and limited entry into the building for anybody who could be an asymptomatic carrier,” Barrett said. “But we weren’t catching anyone between January and March who was an asymptomatic carrier.”
Following the governor’s recent executive order mandating that nursing homes start testing their workers every week, Barrett said the industry will dramatically improve its ability to identify and isolate infections from both asymptomatic and symptomatic carriers.
“Going forward we will achieve much better outcomes with a testing strategy in place, where we didn’t have that in February, March, April and a good part of May,” he said. “ … And it wasn’t because Connecticut nursing homes were wrong — the science, medical and academic community studying COVID didn’t understand that it was transmitting through asymptomatic carriers. We believe that will tell a big part of this story.”
A CT Mirror report contributed to this story

2022 Giving Guide
This special edition informs and connects businesses with nonprofit organizations that are aligned with what they care about. Each nonprofit profile provides a crisp snapshot of the organization’s mission, goals, area of service, giving and volunteer opportunities and board leadership.
Learn more
Subscribe
Hartford Business Journal provides the top coverage of news, trends, data, politics and personalities of the area’s business community. Get the news and information you need from the award-winning writers at HBJ. Don’t miss out - subscribe today.
Subscribe
2024 Book of Lists
Delivering Vital Marketplace Content and Context to Senior Decision Makers Throughout Greater Hartford and the State ... All Year Long!
Read Here-
2022 Giving Guide
This special edition informs and connects businesses with nonprofit organizations that are aligned with what they care about. Each nonprofit profile provides a crisp snapshot of the organization’s mission, goals, area of service, giving and volunteer opportunities and board leadership.
-
Subscribe
Hartford Business Journal provides the top coverage of news, trends, data, politics and personalities of the area’s business community. Get the news and information you need from the award-winning writers at HBJ. Don’t miss out - subscribe today.
-
2024 Book of Lists
Delivering Vital Marketplace Content and Context to Senior Decision Makers Throughout Greater Hartford and the State ... All Year Long!
ABOUT
ADVERTISE
NEW ENGLAND BUSINESS MEDIA SITES
No articles left
Get access now
In order to use this feature, we need some information from you. You can also login or register for a free account.
By clicking submit you are agreeing to our cookie usage and Privacy Policy
Already have an account? Login
Already have an account? Login
Want to create an account? Register
Get access now
In order to use this feature, we need some information from you. You can also login or register for a free account.
By clicking submit you are agreeing to our cookie usage and Privacy Policy
Already have an account? Login
Already have an account? Login
Want to create an account? Register






0 Comments